Table of Contents
Your gut isn’t just a food tube—it’s the foundation of your health. Here’s what actually works, backed by real science.
Table of Contents
Quick Truths: Myths Busted
❌ Myth
- “Stress causes ulcers”
✅ Reality
- H. pylori bacteria and NSAIDs cause 95% of ulcers
❌ Myth
- “Probiotics fix IBS”
✅ Reality
- ACG suggests against probiotics for IBS—try low-FODMAP diet first
❌ Myth
- “Digestive enzymes cure bloating”
✅ Reality
- OTC enzymes aren’t regulated; only proven for specific deficiencies
Irritable Bowel Syndrome (IBS)

IBS affects how your gut moves and feels, without visible damage on scopes
IBS is a symptom-based condition—recurring abdominal pain related to bowel movements, plus changes in stool form or frequency. There’s no visible damage on scopes, which is why tests often look “normal” even when you don’t feel normal. Subtypes include IBS‑D (diarrhea), IBS‑C (constipation), and IBS‑M (mixed). [NIDDK]
What Actually Helps
- Low‑FODMAP diet: A supervised 3‑phase approach (restriction, reintroduction, personalization) helps many with IBS. Don’t stay in restriction mode forever—reintroduction is the point.
- Soluble fiber: Psyllium helps; insoluble fiber (wheat bran) can backfire for some.
- Skip probiotics: ACG suggests against probiotics for global IBS symptoms due to weak and inconsistent evidence across strains.
Gastroesophageal Reflux Disease (GERD)

GERD can cause chronic cough and other respiratory symptoms
Heartburn and regurgitation happen when the lower esophageal sphincter (LES) weakens or relaxes at the wrong time, letting stomach contents backwash into the esophagus.
Risk goes up with obesity, pregnancy, smoking/secondhand smoke, certain meds (e.g., NSAIDs, some antidepressants, calcium channel blockers), and hiatal hernia.
Lifestyle Moves That Actually Help
- Avoid late meals and elevate the head of bed 6–10 inches
- Identify your actual triggers (common ones: chocolate, coffee, peppermint, fatty/spicy foods, alcohol)
- Lose weight if needed—excess abdominal fat is a major risk factor
- Quit smoking and limit alcohol
Peptic Ulcers: The Real Story

Peptic ulcers cause upper abdominal pain that may worsen or improve with eating
🔬 Science Check
The big two causes are Helicobacter pylori infection and regular NSAID use. That’s it for the vast majority of cases. Emotional stress and spicy food aren’t root causes.
Stress-Related Mucosal Disease ≠ Everyday Stress
There is a separate ICU‑level scenario—stress-related mucosal disease—where critically ill patients with risk factors (coagulopathy, shock, advanced liver disease) need short‑term acid suppression to prevent bleeding. That’s not everyday “stress.”
SCCM guidelines focus on ICU patients with specific risk factors, not everyday stress
Inflammatory Bowel Disease (IBD)
Ulcerative colitis and Crohn’s disease are immune‑mediated conditions that inflame the gut lining and can damage tissue over time.
Symptoms include diarrhea, abdominal pain, rectal bleeding (UC), weight loss, fatigue—and they come in flares and remissions.
Causes are multifactorial: immune dysregulation interacting with genes, environment, and microbiome—not “just stress” or diet alone.
⚠️ Important
IBD requires medical management with anti-inflammatory therapies. Diet and supplements are supportive, not primary treatment.
Gastroenteritis (aka “Stomach Flu”)

Hand washing is the best defense against norovirus transmission
Norovirus is the leading cause of vomiting and diarrhea outbreaks in the U.S. It spreads easily and hits fast; most cases resolve in 1–3 days with fluids and rest.
Wash hands well and don’t prep food for others until 48 hours after symptoms stop.
Chronic Diarrhea & Constipation
Chronic Diarrhea
- Definition: ≥4 weeks of loose/watery stools ≥3/day
- Common causes: IBS‑D, IBD, celiac disease, microscopic colitis, bile acid diarrhea, post‑infectious changes, medications
Chronic Constipation
- Definition: Fewer than three BMs/week and/or hard, difficult stools
- Common causes: Low fiber/fluid intake, pelvic floor dysfunction, metabolic/hormonal issues, neurologic disease, medications
What to Try First: Decision Tree
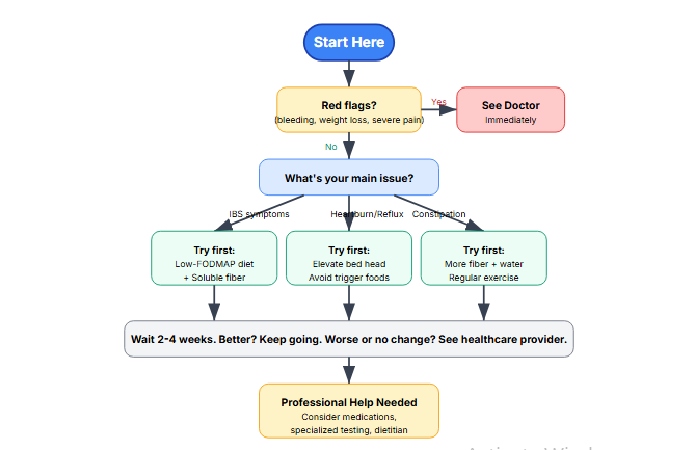
How to Actually Improve Digestive Health
🥗 Diet
- Fiber: 22–34 g/day from whole foods
- Low‑FODMAP for IBS (3 phases)
- Identify GERD triggers
- Stay hydrated
🏃♀️ Lifestyle
- Regular exercise (even walks count)
- Sleep hygiene
- Stress management (CBT, mindfulness)
- Quit smoking, limit alcohol
💊 Medical
- PPIs for GERD when needed
- Anti-inflammatory therapies for IBD
- Targeted medications for IBS
- H. pylori eradication if positive
Supplements: Where Evidence Starts and Stops
Digestive Enzymes
✅ When They’re Essential
Prescription PERT for exocrine pancreatic insufficiency (EPI) from pancreatitis, cystic fibrosis, pancreatic surgery/cancer
❌ OTC “Broad-Spectrum” Claims
Generally not needed in healthy people, not FDA-regulated, claims about “fixing bloating” aren’t backed by robust trials
Probiotics
IBS: ACG Says No
ACG suggests against probiotics for global IBS symptoms—evidence is very low quality and inconsistent across strains
During Antibiotics: Maybe
Can modestly reduce antibiotic-associated diarrhea and C. diff risk; absolute benefit is small (NNT ~65)
IBD: Research Only
Current guidance limits probiotic use to research contexts for Crohn’s/UC. Don’t replace standard therapies
Collagen
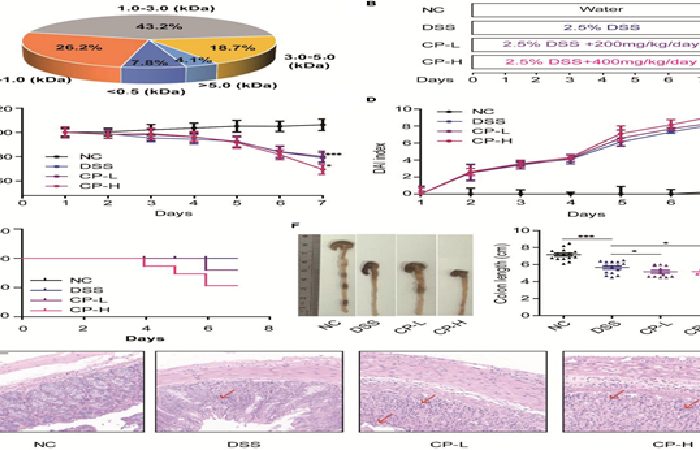
Mouse study showed collagen peptides worsened colitis progression
⚠️ Reality Check
Human gut data are preliminary. One small study suggested less bloating—but no control group and high drop-out.
Meanwhile, a mouse colitis model found collagen peptides worsened inflammation and barrier integrity.
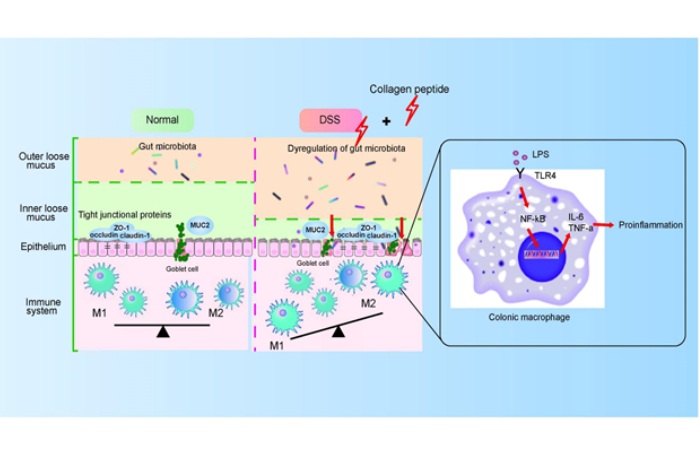
Proposed mechanism: collagen peptides may disturb gut microbiota and trigger inflammation
Bottom line: Don’t recommend collagen for gut healing or IBD management.
Curcumin (Turmeric Extract)
UC Data Exist—As Add-On
RCTs show curcumin added to mesalamine can help maintain remission and aid induction in mild‑to‑moderate UC.
- • Maintenance: 4.7% relapse vs 20.5% on placebo over 6 months
- • Induction: 53.8% remission vs 0% on placebo at 4 weeks
CBD and Cannabis
✅ May Help Symptoms
Pain, sleep, appetite relief reported by some users
❌ No Disease Control
Doesn’t reduce intestinal inflammation or improve IBD course
⚠️ Caution
Heavier/longer use can correlate with worse outcomes (e.g., higher surgery risk in Crohn’s). Should not replace standard therapy.
🚩 Red Flags: Don’t Wait This Out
Seek Care Urgently For:
- GI bleeding: Black/tarry stools, coffee-ground or bloody vomit
- Unexplained weight loss
- Persistent vomiting
- Dysphagia (difficulty swallowing)
- Severe or nocturnal pain
- Any sudden change in symptoms that worries you
Get Evaluated For:
- GERD that doesn’t respond to OTCs/lifestyle changes
- Suspected ulcers or IBD
- Chronic diarrhea or constipation affecting quality of life
Frequently Asked Questions
Is stress a cause of ulcers?
Not typical life stress. The main causes of peptic ulcers are Helicobacter pylori infection and regular NSAID use.
There is a separate ICU-level scenario called stress-related mucosal disease, where critically ill patients with specific risk factors need acid suppression, but that’s not everyday emotional stress.
Should I take a probiotic for IBS?
Current ACG guidelines suggest against probiotics for global IBS symptoms due to very low quality and inconsistent evidence across strains.
Try dietary approaches like low-FODMAP with dietitian guidance first, along with evidence-based medications if needed.
Do digestive enzymes help bloating?
Over-the-counter digestive enzyme supplements are generally not needed in healthy people and aren’t FDA-regulated for dose/potency.
Claims about fixing bloating broadly aren’t backed by robust trials. Prescription enzymes (PERT) are essential for specific conditions like pancreatic insufficiency.
Is collagen good for gut healing?
Human gut data for collagen are preliminary at best. One small study suggested less bloating, but it lacked a control group.
Meanwhile, a mouse colitis model found collagen peptides worsened inflammation. Don’t recommend collagen for gut healing or IBD management.
Does CBD reduce gut inflammation?
CBD may provide symptom relief (pain, sleep, appetite) for some, but evidence doesn’t show it reduces intestinal inflammation or improves disease course in IBD.
It should not replace standard therapy, and heavier/longer use can correlate with worse outcomes.
Quick Disclaimer:
This content is for educational purposes and does not replace professional medical advice. Always consult your healthcare provider for personalized recommendations.
